Connect
SHG Facebook Diabetes Education – Explore Valuable Resources (Click the Facebook link above to learn more).
Diabetes Education

What is Diabetes?
Diabetes is a chronic health condition that affects how your body processes glucose, commonly known as blood sugar. Glucose is a vital energy source for your body, and insulin, a hormone produced by the pancreas, plays a key role in allowing glucose to enter your cells where it is converted into energy.
The Lock & Key concept
The "lock and key" analogy is often used to explain this process. Think of insulin as the key and your cells as locks – under normal conditions, insulin (the key) binds to receptors on your cells (the locks) to "unlock" them and let glucose in. In diabetes, this system doesn't work as it should. In type 1 diabetes, the body doesn't produce insulin (the key is missing), and in type 2 diabetes, the cells may become resistant to insulin (the key doesn't fit the lock properly). This leads to an accumulation of glucose in the blood, which can cause serious health complications if not managed properly.

What is Type 1 Diabetes?
Type 1 diabetes is a chronic condition where the pancreas produces little to no insulin, a hormone vital for regulating blood sugar levels. This autoimmune disease occurs when the body's immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. While its exact cause is not fully understood, factors like genetics and certain environmental triggers may play a role. Unlike Type 2 diabetes, Type 1 typically develops in children, teenagers, or young adults, but it can occur at any age. Managing Type 1 diabetes involves regularly monitoring blood sugar levels, administering insulin through injections or pumps, maintaining a balanced diet, and staying active. Although there is currently no cure, people with Type 1 diabetes can lead healthy, fulfilling lives with proper care and support.


What is Type 2 Diabetes?
Type 2 diabetes is a chronic health condition that affects the way your body processes blood sugar (glucose). It occurs when your body either doesn’t produce enough insulin or doesn’t use it effectively. Insulin is a hormone that helps regulate blood sugar levels, ensuring your cells get the energy they need to function properly. Without proper insulin use, blood sugar can build up, leading to health complications over time. While genetics can play a role, lifestyle factors such as being overweight, inactive, or consuming an unhealthy diet often contribute to its development. Managing Type 2 diabetes typically involves a combination of a balanced diet, regular exercise, maintaining a healthy weight, and in some cases, medication or insulin therapy.
What is Pre Diabetes/ Impaired glucose?
Pre-diabetes is a condition where blood sugar levels are higher than normal but not yet high enough to be classified as type 2 diabetes. A common way to understand how this works is through the "lock and key" analogy. In your body, insulin acts like a "key" that unlocks the "doors" of your cells, allowing glucose (sugar) from your bloodstream to enter and be used for energy. In pre-diabetes, this process begins to break down. Either the "key" (insulin) doesn’t work as well as it should to open the "lock" (cell receptors), or the "locks" themselves become resistant to the key. This is called insulin resistance. If not further investegated and no lifestyle changes occur, pre-diabetes can progress to type 2 diabetes, increasing the risk of associated complications including heart disease, stroke, and other health complications. Fortunately, with early detection and lifestyle changes—like eating a balanced diet, exercising regularly, and maintaining a healthy weight range — it’s possible to manage or even reverse pre-diabetes and keep your cells functioning optimally.

What Is Gestational Diabetes?
Gestational diabetes is a type of diabetes that can develop during pregnancy in women who didn’t have diabetes before. It occurs when the body cannot produce enough insulin to meet the increased demands of pregnancy, leading to higher-than-normal blood sugar levels. While gestational diabetes typically resolves after the baby is born, it’s important to manage it properly during pregnancy to avoid potential complications for both the mother and the baby.
This condition can sometimes be managed through simple lifestyle changes, such as eating a healthy, balanced diet and staying active. In some cases, medication or insulin may be required.
Regular prenatal check-ups and monitoring are crucial for ensuring both mum and baby remain healthy.
If you’ve been diagnosed with gestational diabetes, speak to your healthcare provider about creating a personalised care plan that works for you.
To understand this, think of the "lock and key" concept. Insulin is the key, and it helps unlock the cells (the locks) to let glucose (blood sugar) enter and be used for energy. In gestational diabetes, the body either doesn’t produce enough insulin or the cells become resistant to it, meaning the key (insulin) doesn’t fit the lock properly. This leads to higher levels of glucose in the bloodstream, as it cannot enter the cells effectively. Proper management can help keep blood sugar levels stable and ensure a healthy pregnancy for both mum and baby.




Understanding Familial Diabetes MODY
Familial diabetes MODY (Maturity-Onset Diabetes of the Young) refers to a rare, hereditary form of diabetes caused by a single genetic mutation. Unlike Type 1 or Type 2 diabetes, MODY often develops at a young age, typically before the age of 25, and is not associated with obesity or lifestyle factors. This condition runs in families, with a 50% chance of inheritance if one parent carries the gene mutation. MODY is characterised by impaired insulin production rather than insulin resistance, making its management distinct from other types of diabetes. Early diagnosis and genetic testing are essential for proper treatment, which may include lifestyle adjustments, oral medications, or insulin therapy, depending on the specific MODY subtype. If you suspect familial diabetes MODY in your family, consult a healthcare professional for guidance and tailored management strategies.
Types of Familial MODY Genes
Familial MODY (Maturity Onset Diabetes of the Young) is a rare form of diabetes caused by hereditary genetic mutations. There are several identified types of MODY genes, each linked to specific genetic variations that impact insulin production or regulation. The most common MODY types include HNF1A, HNF4A, and GCK, which account for the majority of cases. Other less common types, such as HNF1B, KLF11, and PDX1, also contribute to the condition. Each type varies in its clinical presentation and treatment approach. Accurate diagnosis through genetic testing is essential to identify the specific MODY gene, enabling tailored management and care.


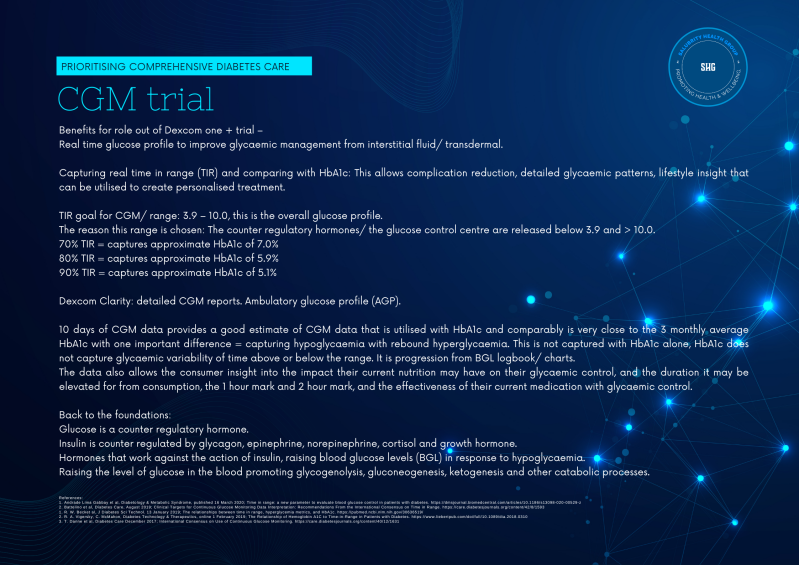
Filling the gap in Primary Care to Diabetes Technology: CGM for T2D & GDM
Dexcom ONE+ Continuous Glucose Monitor Device | Dexcom
Click the link above to check your eligibility, or speak with your Diabetes Educator or General Practitioner to learn more about CGM options.
Take control of your glucose levels, review your results with your GP, Endocrinologist, or Diabetes Educator, and gain valuable insights through the Clarity report.
Create Your Own Website With Webador